NECK PAIN
NECK PAIN

Our neck is an important body part which allows for three-dimensional head movements, while providing anchor to shoulder muscles for upper limb tasks. It has many specialized muscles, and its control is linked to vision, balance and initiation of head, trunk, upper limb and whole body movements. It also a strong structure with lots of nerve receptors to protect our spinal cord, exiting nerves roots and peripheral nerves travelling into the upper limb and blood vessels supplying head and brain.
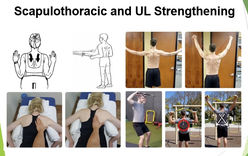
Our neck health is dependent upon regular movements and muscle strength of the neck and upper limb while at the same time caring for general health (physical and psychological).This facilitates a pathway to wellness and functional restoration.


Neck pain is an umbrella term that refers to pain at the back, sides and front of the neck. Neck pain can also happen with pain referring between shoulder blades and into arm, and cause headaches as well. There can be specific causes (specific spinal pathology causing neck pain; e.g. infection, tumor, osteoporosis, fractures, rheumatoid arthritis, nerve compression radiculopathy, myelopathy). Common medical diagnostic labels for not so serious neck pain include: disc degeneration, bulges, prolapses, facet arthropathy, annular tears, spondylosis, stenosis.
Non-specific’ neck pain (i.e. pain not attributed to specific spinal pathology) is by far the most common type of neck pain (e.g. strain or sprain in the absence of pathology. Most ‘non-specific’ neck pain cases settle within few days and respond well to simple conservative management. The mechanism for this type of neck pain typically results from sustained postures ( e.g. prolong neck bending at work, unusual sleeping position or uncomfortable pillow etc.).
The best practice guidelines for the management of ‘non-specific’ neck pain are to perform exercises to preserve and improve neck movements and strength, pace activity, and caring for general physical health (healthy weight, good sleep habits, regular physical activity) / psychological health (stress/ mood). Simple analgesia (paracetamol, anti-inflammatory medications) and pain relieve adjuncts may also be recommended to provide window to chase active recovery.
Physiotherapists are key healthcare providers for conservative neck care, being tasked to prevent persistent pain and disability, and facilitating a pathway to wellness and functional restoration.
OTHER RESOURCES AND INFOGRAPHICS
FREQUENTLY ASKED QUESTIONS
REFERENCES
-
Yu H, Cote P, Southerst D, et al. Does structured patient education improve the recovery and clinical outcomes of patients with neck pain? A systematic review from the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. The spine journal : official journal of the North American Spine Society 2014. [PubMed]
-
Takasaki H, May S. Mechanical diagnosis and therapy has similar effects on pain and disability as ‘wait and see’ and other approaches in people with neck pain: a systematic review. Journal of physiotherapy 2014; 60(2): 78-84. [PubMed]
-
Varatharajan S, Cote P, Shearer HM, et al. Are work disability prevention interventions effective for the management of neck pain or upper extremity disorders? A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) collaboration. Journal of occupational rehabilitation 2014; 24(4): 692-708. [PubMed]
-
Southerst D, Nordin MC, Cote P, et al. Is exercise effective for the management of neck pain and associated disorders or whiplash-associated disorders? A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. The spine journal : official journal of the North American Spine Society 2014. [PubMed]
-
Motor Accidents Authority. Guidelines for the management of acute whiplash-associated disorders – for health professionals. Sydney, 2014. [PDF]
-
Sutton DA, Cote P, Wong JJ, et al. Is multimodal care effective for the management of patients with whiplash-associated disorders or neck pain and associated disorders? A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. The spine journal : official journal of the North American Spine Society 2014. [PubMed]
-
Chaibi A, Russell MB. Manual therapies for primary chronic headaches: a systematic review of randomized controlled trials. J Headache Pain 2014; 15: 67. [PubMed]
-
Sterling, M., et al. (2019). “Physiotherapist-delivered stress inoculation training integrated with exercise versus physiotherapy exercise alone for acute whiplash-associated disorder (StressModex): a randomised controlled trial of a combined psychological/physical intervention.” Br J Sports Med 53(19): 1240-1247 [PubMed]
%20OnPoint%20Enlarged.png)